Cardio-HARTTM
AI Heart Diagnostic System — Fast, Accurate, At the Point of Care
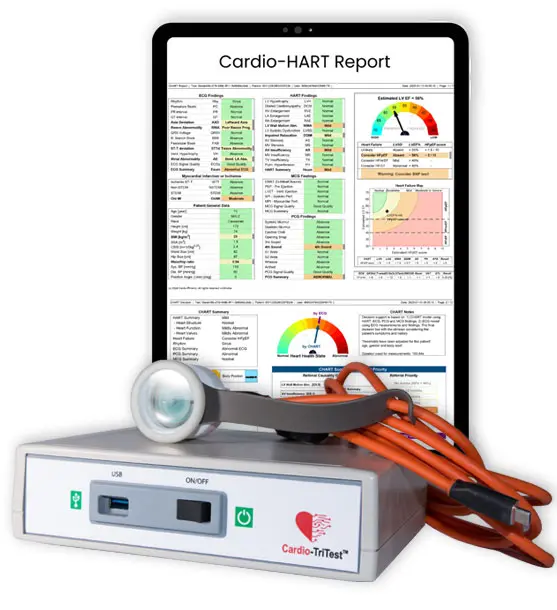
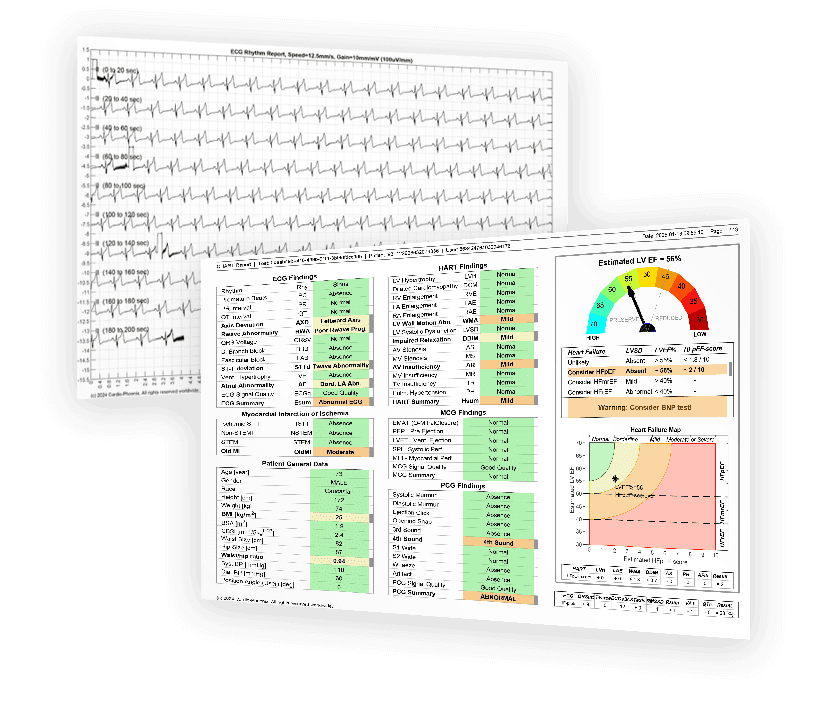
- Detection of HF, HFpEF, HFmrEF, HFrEF valve disease, and structural heart anomalies
- Simpson Biplane levels of LVEF estimation and HF scoring
- Severity information, on Echo and ECG findings
- Structured reports, readable by any clinician—no specialist required
94%
reduction in inconclusive ECGs¹
160%
increase in confirmed diagnoses¹
96%
echo-agreement rate¹
¹ Source: Cardio-Phoenix Multicentre Study (2022); Validation results presented at ESC-HFA 2023;
peer-reviewed in European Heart Journal: Digital Health (2023).
- Cut echo referrals by up to 66%
- Reduce echo waiting lists and clinical backlogs
- Enable same-day triage and improve time to treatment
- Faster diagnosis and follow-up
- More appropriate evidence based specialist referrals
- Echo slots reserved for truly complex cases
- Earlier HF diagnosis
- Faster treatment initiation
- Reduced low-value diagnostics
- Optimized out-patient pathways
- Triggers re-allocable cost savings
Validation Through Real-world Testing
What Happened When HCPs Faced Real Diagnostic Challenges
🧪
Study Methodology
- Venue: 3 cardiology conferences (2024–2025)
London Diabetes & Cardiology Show, London Heart Failure Show, Seville Cardiology Congress
- Use Case: Two inconclusive ECG cases common in GP practice
- Data Provided:
- ECG-only: Traces, AI findings, Measurements
- Cardio-HART: Full CHART Report including ECG + Echo-like data

🔁 Two-Step Survey Protocol
Step 1: Using only ECG
Doctors had 5 minutes per case to:
- Review the ECG, traces, findings and measurements
- Make a diagnosis
- Decision: refer to a cardiologist or treat in clinic
Step 2: Cardio-HART Review
Then, they received the Cardio-HART AI heart diagnostic report for the same case and could revise their decision.
Results
Step 1 – ECG-Only Results
Diagnostic confidence was extremely low
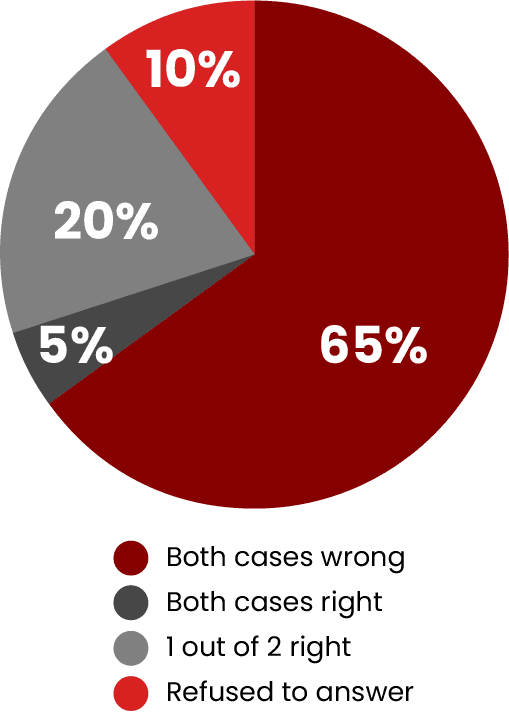
Step 2 – With Cardio-HART
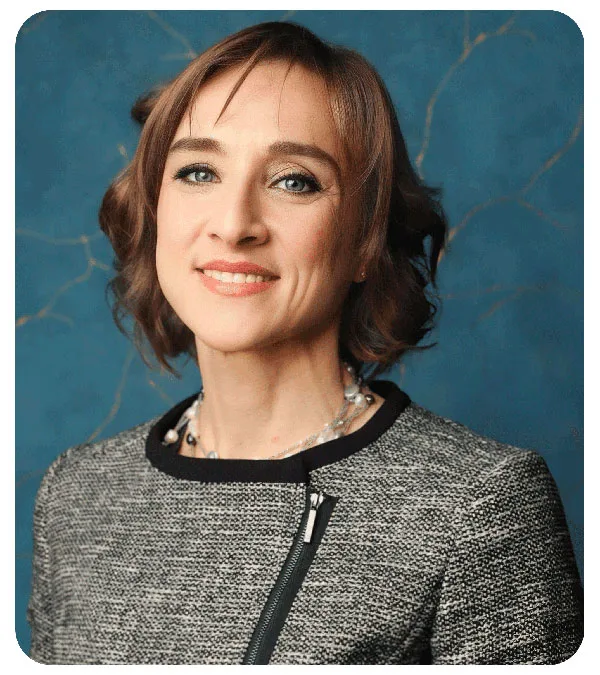
It gets clear answers—fast! That’s why I replaced my standard ECG with Cardio-HART AI heart diagnostic. It gives me everything a standard ECG does, plus it adds echo-level insights–in minutes—helping me detect early signs of heart failure or valve disease so I can take action straight away.
If NHS adopted Cardio-HART at scale, we’d ease pressure on hospital echo departments and make faster, better-informed decisions for patients.
Doctor Teresa Castiello
Cardiology President of Royal Society of Medicine (2023-2025)
ESC cardiomyopathy nucleus and CardioGenomic Council
Prevention Begins at First Contact
1. As declared by the President of Pumping Marvellous a foundation promoting the use of NTproBNP in the UK.
Who it helps. Role-Based Benefits
For General Practitioners
Fits your workflow, improves diagnostic certainty
- Triage confidently with data
- Eliminate uncertainty in inconclusive ECGs
- Start treatment straight away
Discover how Cardio-HART AI heart diagnostic supports GPs –>
For Cardiologists
Streamlines referrals and echo prioritisation
- Better referrals, pre-triaged
- Reduce low-yield echo demand
- Focus on high-value imaging

For Patients
Faster answers, faster care
- One quick test, local clinic
- Immediate results = reassurance
- No more long waits for hospital echo
For Commissioners (ICBs)
Earlier diagnoses saves costs, reduces waiting times and time to treatment.
- Aligned with ICS/NHS Long Term Plan
- Triggers re-allocable cost savings.
- Reduces referral burden, improves access, fosters net-zero