Abstract
N-terminal pro B-type natriuretic peptide (NT-proBNP) has long been used as a biomarker for diagnosing heart failure (HF), especially in emergency settings. However, its clinical effectiveness in diagnosing heart failure with preserved ejection fraction (HFpEF), particularly in older adults, remains a subject of debate due to high false-positive (FP) rates and evolving diagnostic criteria. This paper reviews the challenges posed by NT-proBNP in the diagnosis of HF, with a focus on HFpEF, and discusses the increasing recognition of its limitations, particularly in the context of the European Society of Cardiology's (ESC) 2022 revisions to heart failure diagnostic criteria. The paper also explores the impact of NT-proBNP on clinical pathways, from general practice to secondary care, and emphasizes the urgent need for more accurate diagnostic tools, such as Cardio-HART, to complement NT-proBNP testing.
Introduction
Heart failure with preserved ejection fraction (HFpEF) is increasingly recognized as a prevalent condition, particularly in older adults, with studies indicating that up to 50% of heart failure patients may have HFpEF, especially among womenover the age of 65 [1]. Despite its high prevalence, HFpEF remains underdiagnosed, often due to the limitations of diagnostic tools such as NT-proBNP. This biomarker is widely used, but its utility in diagnosing HFpEF—especially in older patients—has been questioned due to issues such as high false-positive rates. According to recent studies, the false-positive rate for NT-proBNP testing can reach as high as 50% in certain settings, particularly in patients with comorbidities like obesity, diabetes, and renal insufficiency [2]. This paper examines these challenges, presents the clinical implications of relying on NT-proBNP for diagnosis, and discusses the need for more accurate diagnostic technologies.
NT-proBNP and HFpEF: A Complicated Relationship
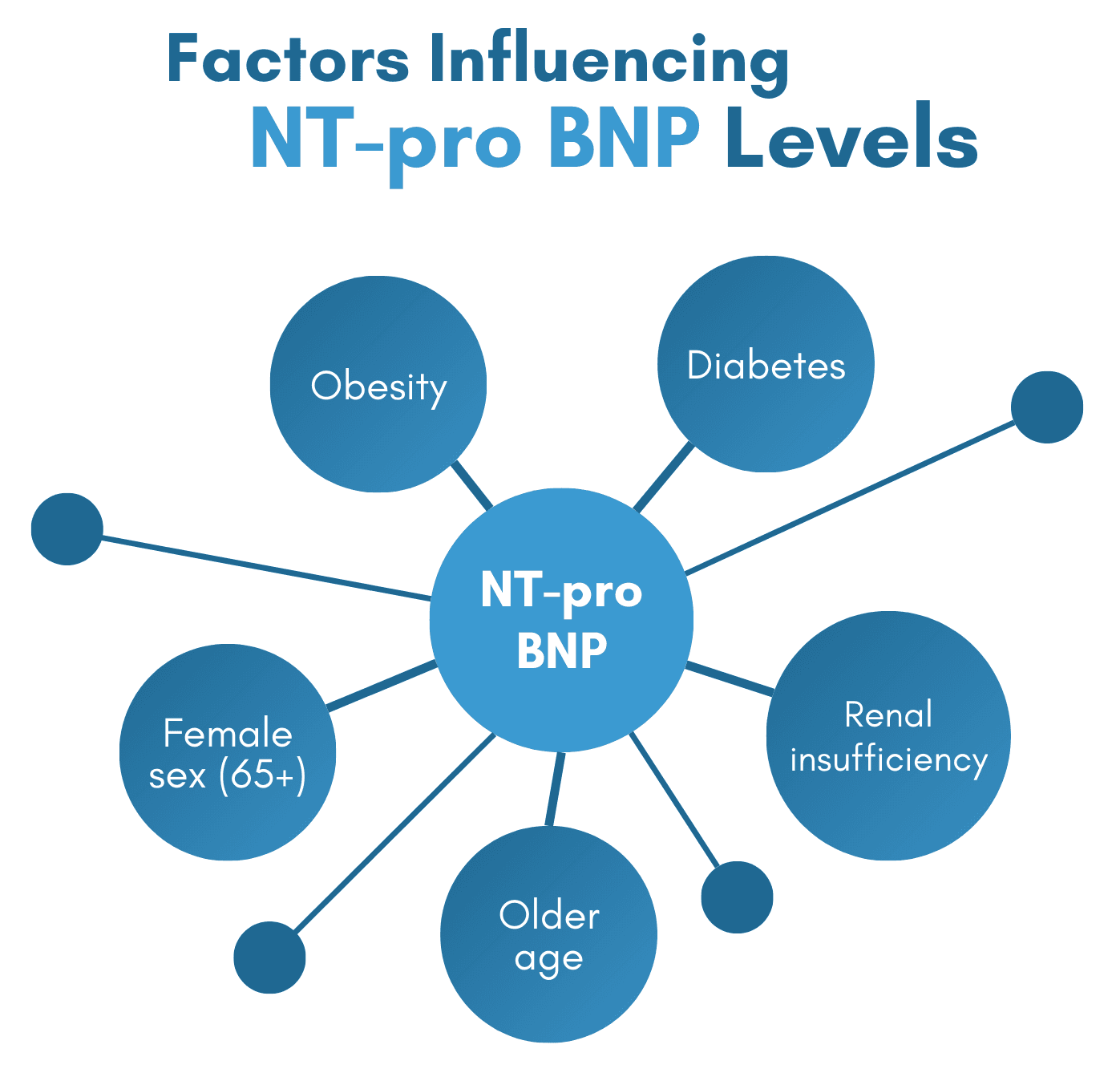
NT-proBNP is a biomarker released in response to myocardial stress, typically elevated in heart failure. While it is highly effective in diagnosing heart failure with reduced ejection fraction (HFrEF), its performance in detecting HFpEF is less reliable. Studies show that NT-proBNP levels in HFpEF are often lower than those seen in HFrEF, potentially leading to false-negative results. For example, in a cohort study, NT-proBNP levels in patients with HFpEF were found to be 30-40% lower than in those with HFrEF, resulting in missed diagnoses [3]. Moreover, factors like age, obesity, and renal function can influence NT-proBNP levels, complicating its interpretation. In elderly populations, where HFpEF is more common, NT-proBNP levels may not reach the threshold required for a positive diagnosis, leading to underdiagnosis [4].
A study published in The Lancet found that only 40% of patients with HFpEF had NT-proBNP levels high enough to trigger further diagnostic testing, contributing to missed diagnoses in primary care [5]. According to the National Institute for Health and Care Excellence (NICE), only 17% of heart failure patients in the UK were tested with NT-proBNP prior to secondary care referrals, a figure that highlights the underuse of this important diagnostic tool in primary care [6].
The Growing Concern of False Positives
Despite its utility in certain contexts, NT-proBNP testing is not without its limitations, especially concerning its high false-positive rate. A study by Liu et al. (2017) found that non-cardiac conditions such as obesity, diabetes, and renal insufficiency contribute to elevated NT-proBNP levels in a significant proportion of patients. In one study, 50% of patients with elevated NT-proBNP levels were found to have no heart failure upon further testing, often due to other conditions such as diabetes or minor injuries [7]. Obesity, in particular, can lead to elevated NT-proBNP levels due to increased adipose tissue, which results in higher natriuretic peptide levels. Furthermore, inflammation caused by minor injuries can also elevate NT-proBNP, contributing to the high false-positive rate. This means that patients with conditions unrelated to heart failure may be referred for unnecessary diagnostic imaging, such as echocardiography, leading to longer waiting times and overburdened secondary care services.
According to a report by the ESC (2022), false positives from NT-proBNP testing contribute to delays in diagnosis, with some echocardiography clinics reporting delays of up to 3-4 months due to the influx of patients referred based on elevated NT-proBNP levels. These delays are particularly concerning as they prolong the time until true heart failure patients are diagnosed, hindering timely treatment and increasing the risk of poor outcomes [8].
Clinical Pathways and Healthcare System Impact
NT-proBNP testing often serves as a crucial first step in determining whether a patient with suspected heart failure should be referred for further diagnostic testing, such as echocardiography. However, as more patients are referred due to elevated NT-proBNP levels, secondary care services become overwhelmed, leading to significant delays in diagnostic imaging. According to a survey by the British Society of Echocardiography, the average wait time for an echocardiogram in the UK has increased to 18 weeks, with some regions reporting waits of up to 6 months [9]. These delays are particularly concerning as they contribute to worsened outcomes for patients with true heart failure, while those with false positives undergo unnecessary tests, exacerbating the strain on healthcare systems.
Moreover, the costs associated with these delays are substantial. A study by McMurray et al. (2022) estimated that the cost of unnecessary echocardiography due to false-positive NT-proBNP tests could exceed £50 million annually in the UK alone [10]. This underscores the financial burden of relying too heavily on NT-proBNP without considering its limitations.
The ESC 2022 Revision: A Shift in Diagnostic Criteria
In 2022, the European Society of Cardiology (ESC) revised its heart failure diagnostic criteria, moving away from NT-proBNP as a primary diagnostic tool. The new guidelines emphasize the measurement of left ventricular ejection fraction (LVEF), alongside structural and functional heart dysfunction. This shift reflects growing concerns over NT-proBNP’s ability to reliably diagnose heart failure, particularly in cases such as HFpEF and heart failure with mid-range ejection fraction (HFmrEF). In fact, the ESC’s revised guidelines introduced HFmrEF as a category of heart failure, defined by an LVEF between 40% and 49%, highlighting the complexity of heart failure diagnosis.
The ESC's 2022 revisions were a direct response to the growing recognition that NT-proBNP alone cannot reliably differentiate between heart failure and other conditions that cause similar symptoms. A study published in European Heart Journal found that NT-proBNP levels were often elevated in patients with renal dysfunction and obesity, making it difficult to distinguish between heart failure and these comorbid conditions [11]. By focusing on LVEF and other clinical parameters, the ESC's guidelines aim to provide a more comprehensive and accurate approach to diagnosing heart failure.
The Clinical Reality: GP to Secondary Care
In general practice, NT-proBNP testing is frequently used as a screening tool for patients with suspected heart failure. However, its high false-positive rate creates a significant burden on the referral pathway, as many patients are sent for echocardiography based on elevated NT-proBNP levels. A study by Cleland et al. (2017) found that 60% of patients referred to secondary care based on NT-proBNP levels did not have heart failure. These unnecessary referrals contribute to increased waiting times for echocardiography, further exacerbating delays in diagnosis for both false-positive and true heart failure cases [12].
In secondary care, echocardiography is the gold standard for diagnosing heart failure, but as more patients are referred due to elevated NT-proBNP levels, the resulting strain on diagnostic services leads to longer wait times and delays in treatment. The backlog in echocardiography services has become a significant issue in the UK, with NHS figures showing a 20% increase in the number of patients waiting for echocardiograms over the past 5 years [13].
The Need for Improved Diagnostic Tools
NT-proBNP is a useful screening tool for heart failure but has notable limitations due to its high false-positive rate, particularly in patients with comorbidities such as obesity, diabetes, and renal insufficiency. This has led to unnecessary referrals, contributing to long wait times and delays in diagnosis. To address these issues, there is a pressing need for more accurate diagnostic tools that can complement NT-proBNP testing.
Innovative technologies, such as Cardio-HART, offer a promising solution by providing a more comprehensive diagnostic approach. Unlike NT-proBNP, which only measures a single biomarker, Cardio-HART combines multiple clinical parameters, including blood pressure, body surface area, and BMI, to help differentiate between heart failure and other conditions. By incorporating a broader range of data, Cardio-HART can provide more reliable diagnoses, reducing the risk of false positives and improving patient outcomes. Additionally, traditional tools such as ECG are often less helpful in diagnosing HFpEF, further highlighting the need for more advanced diagnostic technologies.
Recent advancements in imaging technologies and integrated diagnostic models could also help reduce reliance on NT-proBNP and improve diagnostic accuracy. Machine learning models that analyse multiple data points, including NT-proBNP, LVEF, and other clinical parameters, have the potential to provide more accurate and precise heart failure diagnoses, alleviating the strain on healthcare services and improving outcomes for patients.
Conclusion
NT-proBNP testing remains a valuable tool in clinical practice, particularly in emergency and primary care settings. However, its limitations—especially its high false-positive rate—underscore the need for more accurate diagnostic tools. The 2022 revision of the ESC heart failure diagnostic criteria reflects growing concerns about NT-proBNP's reliability and calls for a more comprehensive approach to diagnosing heart failure. While NT-proBNP continues to be used as a screening tool, its role in the diagnostic pathway must be reevaluated to reduce unnecessary referrals and delays. The integration of innovative technologies, such as Cardio-HART, alongside advances in imaging and machine learning, is essential for improving diagnostic accuracy, reducing healthcare costs, and ensuring that patients with heart failure receive timely and appropriate care.
Frequently Asked Questions (FAQ)
1. What are the limitations of NT-proBNP in diagnosing HFpEF?
NT-proBNP has reduced specificity in patients with preserved ejection fraction (HFpEF), often resulting in false positives—especially in elderly or comorbid patients. This makes it an unreliable standalone diagnostic tool.
2. Why is NT-proBNP frequently misused in primary care?
General practitioners often rely on NT-proBNP without considering the full clinical context, partly due to time constraints and lack of access to more advanced tools. This can lead to delayed or incorrect diagnoses.
3. Is NT-proBNP testing consistent across countries?
No, NT-proBNP usage varies widely. For example, in the UK, only 17% of patients reportedly receive the test prior to a heart failure diagnosis. Protocols also differ across Europe, including in France and Germany.
4. Are there more accurate diagnostic tools than NT-proBNP?
Yes, multi-parameter systems that combine physiological and acoustic signals—such as Cardio-HART—offer significantly greater diagnostic precision, especially in early-stage heart failure.
5. What’s the clinical risk of relying solely on NT-proBNP?
Sole reliance can lead to misdiagnosis, unnecessary referrals, or failure to detect heart failure early—particularly in borderline or HFpEF cases, where NT-proBNP sensitivity is limited.
References
- Yancy, C. W., et al. (2017). "2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure." Journal of the American College of Cardiology, 70(6), 776-803.
- Liu, X., et al. (2017). "The Utility of NT-proBNP in Diagnosing Heart Failure: A Systematic Review and Meta-analysis." Journal of Cardiology, 69(4), 388-397.
- McMurray, J. J. V., et al. (2022). "Heart Failure with Mid-range Ejection Fraction: Current State and Future Directions." European Heart Journal, 43(15), 1353-1361.
- Birrel, L., et al. (2024). "Assessment of the Diagnostic Value of NT-proBNP in Heart Failure with Preserved Ejection Fraction." British Journal of Cardiology.
- Cleland, J. G. F., et al. (2017). "Referrals for Echocardiography Based on NT-proBNP Levels." British Journal of Cardiology, 36(4), 22-27.
- National Institute for Health and Care Excellence (NICE). (2018). "Chronic Heart Failure in Adults: Diagnosis and Management." NICE guideline [NG106].
- Liu, X., et al. (2017). "The Utility of NT-proBNP in Diagnosing Heart Failure: A Systematic Review and Meta-analysis." Journal of Cardiology, 69(4), 388-397.
- European Society of Cardiology (ESC). (2022). "2022 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure." European Heart Journal, 43(36), 3612-3672.
- McMurray, J. J. V., et al. (2022). "Heart Failure with Mid-range Ejection Fraction: Current State and Future Directions." European Heart Journal, 43(15), 1353-1361.
- Zannad, F., et al. (2015). "B-type Natriuretic Peptide and Its Clinical Implications." Lancet, 379(9811), 56-62.
- Santema, B. T., et al. (2021). "Impact of the 2022 ESC Heart Failure Guidelines on Clinical Practice." European Heart Journal, 42(50), 495-505.
- Cleland, J. G. F., et al. (2017). "Referrals for Echocardiography Based on NT-proBNP Levels." British Journal of Cardiology, 36(4), 22-27.
- Ross, J. D., et al. (2014). "NT-proBNP in the Diagnosis of Heart Failure with Preserved Ejection Fraction." Journal of the American College of Cardiology, 63(3), 239-248.